Ch 2 - Literature Review
This page summarises some of the sections of the literature review in Chapter 2 of the thesis. We've included only some of the parts of that long section from the full file. You can view the complete chapter in the full thesis file. Remember this chapter introduces some of the concepts and the ideas behind the research that was done in the 12 different studies of this project.
Role of Cardiac Rehabilitation
Preventive approaches to healthcare have emerged as central features in many areas of modern medicine. In no area of healthcare is this more obvious than in the management of cardiovascular disease (CVD). The effectiveness of preventive strategies in addressing CVD incidence, prevalence, and burden on the individual and social level, has seen cardiac rehabilitation (CR) become recognised as an important secondary prevention strategy in the management of CVD in Australia and abroad.
Large studies have shown that CR exercise interventions can reduce the risk of death following a major cardiac event by around 25-30% [1]. A large review [2] comparing exercise only, diet only, and combined interventions on diabetes incidence and risk factors concluded that while each type of intervention similarly decreased diabetes incidence, significant improvements in weight, BMI (body mass index), and waist circumference were demonstrated by the combined exercise and diet intervention than either type of intervention in isolation.
Guidelines for CR Practice
National and international strategies relating to prevention of CVD have developed into modular recommendation frameworks. CR programs aim to support and shorten recovery periods following an acute cardiac event, promote long-term prevention strategies, encourage positive behaviour change and self management, and promote compliance with medications and professional advice [3]. The scope of CR extends from phase one or inpatient services (mobilisation, education and counselling) to comprehensive outpatient rehabilitation (phase two) and long-term maintenance (phase three) programs.
The defined core group of presentations for which CR is currently recommended includes ischemic heart disease and acute myocardial infarction (MI), post-revascularisation surgeries (angioplasty, stent, coronary artery bypass graft or CABG), stable or unstable angina, and controlled congestive heart failure (CHF). Whilst patients with increased risk factors such as hypertension, hypercholesterolemia, or diabetes may also be referred to outpatient CR, the core group of presentations mentioned form the main focus of recommendations in the current CR framework [3].
Variability in Current CR Practice
Outpatient CR programs can contain significant differences in terms of programming, access, and resources. Thus outcomes in CR settings are quite variable, and it is important to consider the potential scope for this variability. Automatic referral of relevant patients to outpatient CR programs in the US, for example, lagged slightly behind the implementation of the measure in Australia [4]. Patient referral to an appropriate CR program is one of the key requirements in an effective CR framework. However, even with enhanced referral in Australia, patient compliance remains a concern. Across the Hunter New England area in NSW during the last six months in July 2007 for example, only 48% of patients referred to a CR program went on to enrol, with just 35% of all those referred going on to complete an outpatient program [5].
Practitioner concordance with best practice standards is another potential contributor to CR outcome variability. A review of concordance to national guidelines within the inpatient CR setting in Australia [6] found that concordance with different areas of the inpatient guidelines in Australia varied considerably. New approaches to this issue in outpatient CR are emerging, with computerised decision-support systems shown to be useful in enhancing practitioner concordance [7]. Recent health planning suggests that outpatient CR programs will also vary in length, type and content based on patient needs (which is ideal) as well as resource availability [5]. Based on current CR guidelines locally [3], outpatient CR should comprise a minimum of six sessions, either once per week (therefore giving a program duration of six weeks) or twice per week (yielding a minimum recommended duration of three weeks).
However such recommendations vary significantly from the timeframes of many published reports, and studies reported in the literature often utilise training programs of longer periods. One protocol [8] utilised a three-month (12 week) program, with three sessions per week of endurance training (ET), when reporting on pulmonary efficiency and heart rate recovery benefits of this modality. The ELVD-CHF study [9] utilised a six month (24 week) intervention program when reporting on the LV-remodelling benefits of ET in CHF patients. Thus comparisons of intervention outcomes between clinical practice and research investigations may be an added confounding factor in the interpretation of any variability in outcomes. Another factor likely contributing to outcome variability in outpatient CR relates to the non-specific nature of current recommendations with regard to clinical considerations such as patient classification, exercise assessment and prescription, as well as psychosocial factors including motivation. Varibaility in these dimensions of intervention programming lead to a greater range of programming options and differences.
Major Risk Factors for CVD
Many of the presentations attending outpatient CR are closely associated with atherosclerosis and endothelial cell dysfunction. Endothelial dysfunction and cell injury are thought to be the initial stages of the pathogenesis of atherosclerosis. Among the potential triggers of endothelial cell injury are risk factors such as age (especially women over 55), family history, obesity, hypertension, smoking, dyslipidemia, low HDL, and diabetes [10].
The most comprehensive longitudinal research on cardiovascular disease risk factors is known as the Framingham study [11]. This study was begun in 1948, and many updates to the findings have been published since. Figure 1.1 below summarises the acknowledgement of individual risk factors in the form of a timeline. Many other independent studies have also confirmed the impact of these same risk factors. The SHIELD study [12] confirmed that patients with atherosclerosis were at a higher risk (25%) of a serious cardiac event. Data from the NOMAS study [13] reinforced the fact that LDL in particular may be strongly associated with carotid plaque.
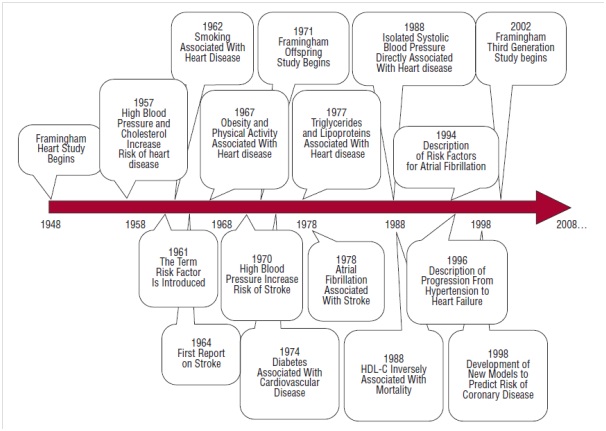
Figure 1.1 - Timeline of major milestones during the Framingham study.
Source: O’Donnell & Elosua, 2008.
Importance of Met-S
The impact of different combinations of various metabolic conditions on cardiac presentations and CR outcomes necessitates a discussion of Metabolic Syndrome (Met-S). This is particularly true since the prevalence of Met-S in an American population of CR patients [19] was more than twice that in the general population, for example. Met-S may at present be defined as a cluster of conditions including hypertension, central obesity, low HDL-cholesterol, high-LDL cholesterol, as well as increased serum triglycerides and fasting blood glucose [20-22]. However Met-S definitions are numerous. A prospective study [23] of patients in Italy with intermittent claudication, with or without Met-S suggested that the International Diabetes Federation (IDF) definition of Met-S, but not the ATP-III criteria, may predict increased cardiovascular risk in patients with symptoms of intermittent claudication typical of peripheral vascular disease (PVD). Given that three of five conditions are required to diagnose Met-S based on either the ATP-III or IDF criteria (with ethnicity-specific waist circumference mandatory in the IDF criteria), the authors point out that there are 16 possible combinations of Met-S under the ATP-III criteria and 11 based on the IDF framework.
Defining Met-S
Emerging opinions on Met-S classification seems to suggest that the ATPIII criteria, in both the original and revised forms, may not be reliable. For example, the results of the RIVANA study from Spain suggest that Met-S (as defined by the original ATPIII criteria) is not better than its individual components in predicting cardiovascular risk (carotid stenosis, increased LV mass in older community-dwelling persons over 65 years [26].
However, females with Met-S and younger than 65 showed an elevated risk of LV hypertrophy, but this was not the case in males where abdominal obesity was a better predictor. The INTERHEART study [27] of patients from 52 different nations also suggested that Met-S was no better as a predictor of MI than its components like DM and hypertension (based on the revised ATP III criteria). Findings of the Tehran Lipid and Glucose (TLG) study of patients (n = 4018) followed up for 6.7 years seem to confirm the results of the RIVANA and INTERHEART studies [28]. However in the TLG study, the 2003 ADA criteria for defining diabetes were tested against the revised ATP-III criteria for Met-S, concluding that Met-S was no better a predictor of CVD risk than diabetes.
Links between Met-S and CVD
Some studies have established a differential disease risk associated with Met-S based on gender. An investigation [32] involving patients with CAD concluded that Met-S was a more reliable predictor of reduced outcomes in females than in males, following an intensive 3-week (6 days per week, 2 sessions per day) rehabilitation program. A review published the same year [33] also highlighted the potential associations of individual Met-S component conditions (i.e. abdominal obesity, hypertension, dyslipidemia, and insulin resistance) and increased CVD risk in women. Thus whilst studies [25] may report a higher prevalence of Met-S component conditions in males, most investigations also report a differentially higher risk of CVD in females associated with Met-S. One study [34] has suggested links between Met-S and future risk of CAD in men as opposed to stroke in women. These findings together reinforce the need to consider gender as in the retrospective studies (Chapters 4-13).
The majority of studies on the impact of Met-S on CAD and PVD risk in fact report strong links. One recent meta-analysis [35] of patients with Met-S investigated the associated risk of CVD and CVD mortality, MI, stroke, and all-cause mortality. Data from this study shows that there may be a much higher risk of these events for those with Met-S. Another more recent study [36] also concluded similarly, showing that MetS may be linked to abnormal left ventricular (LV) structure and function. The results of the Isfahan Cohort Study [37] suggest that Met-S and IHD risk may be closely associated in the Iranian study population followed for 5 years. More recently in Australia, the results of the Dubbo study [38] demonstrated that Met-S may be a genuine contributor to CVD risk, independently of its component conditions. Thus the metabolic comorbidities, MI history and central cardiovascular comorbidities comprise elements of both the retrospective reviews and the patient classification in the NICER pilot (refer to Chapter 3).
Role of Exercise and Diet
Since many of the risk factors for the development of CVD and Met-S are lifestyle-related, it is no surprise that simple lifestyle modifications including diet, weight reduction and exercise [21] are standard components of CR programs. Large meta-analyses [2] have shown that exercise and proper diet together can significantly reduce the risk of diabetes in those with Met-S. Dietary changes alone, however, were shown to be insufficient in delivering significant CVD and Met-S risk reduction. Studies have shown that the glycaemic load (GL) and the glycaemic index (GI) of ingested food directly affects short-term serum glucose and insulin levels [62].
However once factors such as hypertension, history of cardiovascular disease, and physical activity have been accounted for, dietary GI and GL may not be significantly associated with mortality in patients with a history of cardiovascular disease [63]. Achieving adequate glycaemic control requires long-term effective self-management. Group based education interventions to enhance self-management of type 2 diabetes have been shown to significantly reduce fasting blood glucose, HbA1c levels, blood pressure and body weight [64], and thus CR programs which include self-management components aiming to establish long-term therapeutic lifestyle changes including diet and exercise may prove more effective than those without these central points. On this basis, home exercise advice and basic healthy diet support are both elements included within the key-point educational program included within the NICER intervention (refer to Chapter 3 Methods for the educational program details).
The Need for Patient Classification in CR
Given the discussion of Met-S and comorbidities thus far, we can see that the range of presentation attending CR are usually widely varied. The benefits of exercise on all of the component conditions of Met-S [65] have been reported in various studies (as will be discussed later in more detail). However, the HyperGen study [54], as perhaps a follow-up to the Strong Heart study, demonstrated that the partial reversal of individual Met-S components was not associated with improvements in central cardiovascular parameters such as left ventricular hypertrophy (LVH). Based on such evidence, it may be important to develop a CR approach that addresses all of the Met-S component conditions if the program is to successfully minimise the risks associated with the syndrome. This would be in addition to the consideration of primary cardiac presentations leading to patient referral to CR. In order to develop such a program, one might begin with a risk stratification and patient classification system, facilitating appropriate planning of CR interventions for the individual patient. Such a patient classification system is thus far lacking in clinical practice, and the Cardio-Met classification framework included in the NICER intervention (incorporated also into the exercise prescription elements) is one potential model for such a system.
Exercise Modalities in CR
Current CR guidelines recommend patients should aim to exercise for a total of thirty minutes on most or all days of the week at a low to moderate intensity [3]. Moderate intensity activity is defined subjectively here as activity that causes a moderate, noticeable increase in the depth and rate of breathing while allowing the subject to continue talking comfortably. A recent review [66] summarises the evidence for the benefits and risks of exercise in patients with CHF (i.e. those with a compromised low LVEF), with CHF itself considered important in the present discussion given the relative compromises in LVEF (of varying severity) commonly seen in many patients in clinical practice. While not all patients in CR would be classed as having CHF, compromises in LVEF and CHF present important comorbidities in CR. Exercise has been shown to improve functional capacity and resting physiology, and can help attenuate the progression of left ventricular dysfunction typically seen in CHF. The most commonly applied and discussed modalities in CR contexts are aerobic endurance training (ET) and resistance training (RT). Most of the current recommendations however incorporate primarily aerobic training, and more specifically ET as the “gold standard” of exercise prescription in outpatient CR programs.
One of the recent modalities to trigger debate within clinical contexts is interval training (IT). Published results [69] have suggested that IT may improve the control of central sleep apnoea in CHF patients, likely through an improvement in respiratory drive. In fact IT was subsequently shown to improve respiratory drive at rest and at peak exertion in CHF [70]. The DANSUK study [71] demonstrated that ET is able to lower blood pressure and HbA1c in patients with T2DM, in addition to aerobic capacity improvements. Later research [72] demonstrated that ET can attenuate arterial stiffness in men with and without Met-S. However not all published findings relating to exercise and the potential improvements in central cardiovascular function have been positive.
One protocol [73] combining both ET and RT concluded that their approach did not produce significant central improvements. Around this time, the use of RT in CR settings (and particularly with CHF patients) was being thoroughly debated in the literature with some negative opinions [74]. Another study [75] suggested that a combination of RT and ET may be ineffective in enhancing BGL control in type-1 DM patients. Later research and reviews have suggested that the timing of the introduction of RT within the overall CR program can significantly impact the central improvements achievable [76]. However RT can deliver significant benefits to CR patients if correctly applied. Older women with disabilities had earlier been shown to respond to light RT exercise, with improvements in physical function, strength and six-minute walk test [77]. Several studies have demonstrated the usefulness of RT in CR settings, leading to the AHA recommendations [78] that RT form a component of CR to consolidate on the improvements possible with ET alone. More recent evidence [79] has suggested that RT may reduce cholesterol levels in DM patients. The most recent position statement on exercise in CHF patients released by Exercise & Sports Science Australia [80] also recommends a combination of light-moderate ET and light-moderate RT.
Pathology-Specific Exercise in CR
A set of pathology specific protocols covering clinical exercise prescription in outpatient CR (encompassing all of the available clinical modalities) has not yet been presented. For some time authors [74] have argued this point with respect to guidelines internationally, confirming that some form of clinical CR exercise prescription protocols are necessary. For example, an interesting point discussed by one of the recent meta-analyses [76] was that studies which combined ET and RT did not report significant improvements in LV function. Elevated systolic and diastolic filling pressures and LV wall stress associated with RT, as well as the underlying reduction in contractility and preload reserve in patients with a compromised LVEF are likely contributors to these observations. Therefore based on such evidence, in prescribing exercise to CR patients, it may be necessary to exclude RT during the initial phase of outpatient rehabilitation, focusing primarily on attaining the maximum possible central improvements in LV function instead.
Based on this (untested) hypothesis, RT may then be added to a patient’s CR exercise program at a later stage to further improve peripheral function. Flexible yet standardised, condition-specific protocols which aim to apply a range of modalities and more effective dimensioning of exercise (including a “phase” dimension) are thus needed. Given this, the hypothesis for the NICER intervention tested herein (Chapter 15) includes a novel patient classification system (i.e. Cardio-Met classification) which is used as one of the dimensions for prescribing a combination of aerobic ET and IT exercise.
Measuring Functional Capacity
Outcome assessments in clinical CR practice tend to be at either of two intensity extremes. At one extreme are maximal intensity assessments such as maximal exercise stress testing (EST). Authors [100-103] have clearly demonstrated the prognostic value of EST findings in clinical CVD patients. Functional capacity, chronotropic incompetence, and cause of termination of the EST, respectively, were shown by these investigators to be good predictors of cardiovascular risk. Whilst EST protocols usually utilise treadmill testing, protocols using the cycle ergometer [104] have also been validated. Cardiopulmonary exercise testing (CPET) may also be applied in CR settings, and combines standard EST with measures of pulmonary function. As explained by one author [105], CPET defines absolute measures of cardiopulmonary exertion in terms of metabolic equivalents or METs. By definition, 1 MET of caloric expenditure corresponds to a VO2 of 3.5 mL/kg/min, the resting level of oxygen consumption of a healthy 70 kg man. A person during exercise consumes multiples of this resting VO2 value, and this measurement is given as the absolute measure of exertion.
For some time though, investigators [105, 106] have argued against the use of high workload increments and extreme durations such as those applied in the Bruce protocol, as such protocols may not represent true steady-state physiological function. Others [107] demonstrated that a 1-minute protocol is better than a 3-minute protocol when measuring VO2. Based on the evidence, the need for smoother transition between stages to achieve stable, proportionate responses for the longest duration possible seems clear. Such opinions are common amongst those advocating the use of testing methods other than maximal EST in general outpatient CR practice.
The six-minute walk test (6MWT) is a sub-maximal test commonly applied in outpatient CR settings. The usefulness of the 6MWT as an outcomes measure in older patients, as well as patients immediately post-surgery [108] and those with moderate-severe limitations [109-111] has been extensively reported. Thus the 6MWT may be feasible in the assessment of functional capacity and clinical outcomes, or prescribing exercise, in patients who are symptom-limited or less mobile. Symptom relief may also be well represented by the 6MWT [110] especially in patients who demonstrated physiological stress symptoms during a baseline 6MWT. However, some of these studies also demonstrated the unreliability of the 6MWT to adequately represent functional capacity changes in more capable and less symptom-limited patient groups. Therefore given such evidence above relating to maximal and sub-maximal outcomes assessment in CR, the hypothesis for the NICER model includes the novel effective functional capacity (EFC) sub-maximal assessment protocol designed specifically for the needs of outpatient CR settings.
Clinical monitoring (i.e. the observation and noting of specific patient physiologic parameters during exercise) is a matter rarely discussed in scientific literature and guidelines addressing CR patients. For example, the current CR recommendations locally [3] address basic observations during exercise such as symptoms pre- and post-exercise, rate of perceived exertion (RPE), heart rate (HR), blood pressure (BP) and respiratory rate (RR). With the exception of this advice, little other guidance is available in relation to clinical monitoring. Some studies have also highlighted the potential application of some of the measurements taken during the recovery period [8, 112, 113]. Such measurements though are applied with considerable variability in clinical practice, and no standardised CR clinical data-set is available at the time of this writing. The novel clinical aerobic periodisation (CAP) planning tool included within the exercise prescription framework of the NICER pilot study allows the recording of specific physiologic observations (i.e. heart rate, blood pressure and respiratory rate), which are relevant measurements in both exercise assessment through the EFC protocol and monitoring patients during exercise sessions.
Functional Breathing Training (FBT)
Given the central cardiovascular limitations to exercise capacity in CR patients already discussed, it is important to also consider respiratory function. Indeed some authors have argued that exercise-induced bronchoconstriction is common in many people, leading to shortness of breath during exertion [114] and that in patients with compromised LVEF such as in cases with CHF, exercise intolerance and abnormal respiratory patterns are characteristic presentations. Furthermore, both the intolerance to exercise and abnormal breathing were found to be worse with increasing CHF severity [115].
Several approaches have been investigated to address respiratory limitations during exercise. Stepwise-paced breathing (SPB), where the RR is varied based on specific, slow time intervals, reduces BP during exercise in healthy individuals [116]. A small study in hypertensive patients suggesting that slow breathing training (SBT) was able to modify some of the central mechanisms regulating cardiovascular function (i.e. the pressor response), with enhanced recovery of both SBP and HR post-exercise [117], while another group [118] showed that device-guided SBT was able to improve exercise capacity and systolic heart function, as well as diminishing sleep disturbances in CHF patients. The novel functional breathing training (FBT) technique, incorporated into the NICER intervention model being tested herein, was developed to facilitate enhanced breathing during exercise in CR patients. It is designed to be applied simply, and paces the patient’s breathing based on their own inhalation as a timing stimulus to breathing during exercise (refer to Chapter 3). The essential feature of FBT is a trained and deliberate shift in respiratory pattern during exercise, moving from the 1:1:1 inhalation:exhalation:pause ratio typical at rest [119] to a 1:2 inhale:exhale ratio, with the pause eliminated and the focus being on deep full breaths throughout. The primary purpose of FBT is to facilitate better breathing patterns and thereby enhance gas exchange, particularly in patients with abnormal breathing on exercise common in CR patients, particularly those with compromised LVEF [115].
Patient Self-Efficacy, Goal-Setting and Empowerment
Factors such as a history of inadequate exercise, bad exercise experiences, and low self-efficacy (in particular low task self-efficacy), as well as health history, may form major barriers for many patients in outpatient CR [131, 133]. These factors have been included as part of hypothesis 1 of the novel BARE-Q study herein (Chapter 14), tested as part of the NICER intervention. Given the complexity of presentations within these patients, an appropriate solution to reduced adherence may involve more specifically targeted psychosocial interventions. One group of investigators [121] showed that the educational needs of patients in CR comprise mainly a need for advice on self-management strategies and information regarding their health status. Therefore the patient education program and the Motiv-8 motivational framework it is built upon (both novel inclusions in the NICER intervention pilot study) focus on encouraging patient self-efficacy directly as well as their own perceptions of this. Stress and anxiety may also serve as barriers to both the initiation and maintenance of an exercise program [134]. Therefore it may be important to emphasise these factors when formulating patient education and interaction strategies. Indeed patient perceptions of barriers to adherence, including all the above, form the focus of the hypotheses of the BARE-Q study (Chapter 14).
Goal-setting is vital in affecting health behaviour change. Collaborative goal-setting [137] appears to be potentially important as an ongoing focus of the CR program to further enhance adherence. Through effective action and contingency planning [138], maintenance self-efficacy may be enhanced. The bargaining process [139] presents CR practitioners with an opportunity to emphasise the need for effective self-management, and develop realistic objectives as part of expectations-management utilising goal setting. Furthermore, it is important to regularly review the patient’s goals as these may change over time to affect motivation, especially in previously sedentary patients. The novel key-point, multi-week design of the patient education program used in the NICER pilot was developed to facilitate such follow-up and provide collaborative goal-setting opportunities between patients and CR clinicians.
